Plant molecules show promise in priming the antibiotic pipeline
Researchers from several MSU departments are poised to tackle the antibiotic resistance crisis from a different angle — one that aims to disarm the pathogens, as well as destroy them.

Antimicrobial resistant (AMR) pathogens are the largest cause of hospital deaths in the United States, occurring at a rate of 23,000 a year with an additional 2 million illnesses.* And they are gaining even greater strength in what are called “superbugs” – bacteria resistant to all antibiotics on the market.
Now, researchers from departments in the College of Natural Science (NatSci), the College of Veterinary Medicine (CVM) and the College of Agriculture and Natural Resources (CANR) are poised to tackle the AMR crisis from a different angle – one that aims to disarm the pathogens, as well as destroy them.
Supported by an MSU Foundation Strategic Partnership Grant, the researchers are fundamentally changing the ways to control infections, and even cancer, by turning to nature.
Plants, with millions of years of evolution against infections and pathogens, contain some of the most diverse antimicrobial, bioactive enzymes on the planet. These small molecules show great promise to deliver critically needed chemical diversity in pharmaceuticals.
During the past decade, plant scientists including Bjoern Hamberger, MSU assistant professor in the Department of Biochemistry and Molecular Biology (BMB), have learned how to decipher and combine the plant molecules with new synthetically produced substrates to produce plant-inspired chemicals that bacteria have never encountered and therefore, have no resistance to them.
Rick Neubig, professor and chair of the Department of Pharmacology and Toxicology, arrived at MSU six years ago from the University of Michigan with the goal of establishing a drug discovery program. His leadership and vision have brought scientists from across campus together to build and take charge of cutting-edge facilities at MSU, including the Assay Development and Drug Repurposing Core (ADDRC) – a facility used to test, find and house the small molecules that show promise in the antimicrobial resistance assays.
“The ADDRC assists MSU researchers with bridging the drug discovery gap that often exists between their basic research and preclinical drug development,” Neubig said. “It provides expertise in adapting biological and biochemical bench-top assays into high throughput screening (HTS)-compatible assays with the goal of identifying chemical probes to further interrogate a particular biological process or potential leads for drug development.”

The campus-wide resource is directed by Tom Dexheimer, a biochemist in the MSU Department of Pharmacology and Toxicology.
“It provides expertise in adapting biological and biochemical bench-top assays into high throughput screening (HTS)-compatible assays with the goal of identifying chemical probes to further interrogate a particular biological process or potential leads for drug development,” Neubig said.
Edmund Ellsworth, also a professor in the Department of Pharmacology and Toxicology, is another key player in AMR development at MSU. He directs the Medicinal Chemistry Core (MCC), a campus-wide facility that provides investigators with expert consultation on all aspects of the preparation, purification, absorption, distribution, metabolism and excretion, and physical properties of chemical matter.
“The MCC can take the plant-inspired molecules discovered by researchers and optimize them – make them viable to get into animal studies or even, ultimately, to humans,” Neubig explained.
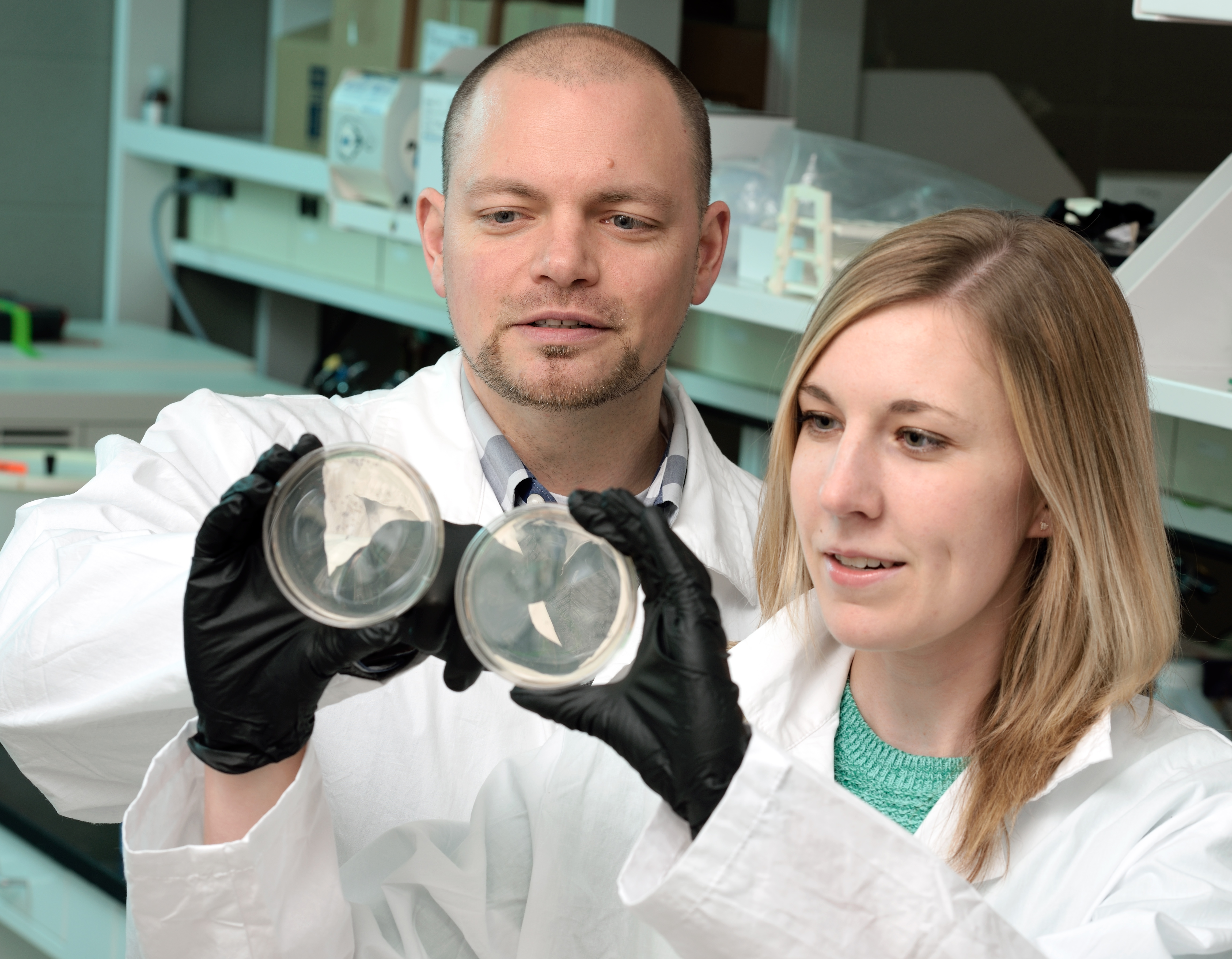
Two leading scientists in the MSU Department of Microbiology and Molecular Genetics (MMG), Victor DiRita, Rudolph Hugh Endowed Chair in microbial pathogenesis, and Neal Hammer, assistant professor, are using the world-class drug discovery facilities to fuel their research.
“We are moving toward precision-based targeting where we discover how the bacteria function in order to disarm them, not necessarily to kill them,” said DiRita, whose lab studies the Gram-negative bacteria devastating hospitals known as Carbapenem-Resistant Enterobacteriaceae (CRE). “This is smart and targeted – this is a laser beam, not a sledgehammer.”
DiRita’s lab will sift through the library of plant-inspired compounds at the ADDRC to identify those that limit in vitro growth of CRE, then target the pathways that lead to colonization of the bacteria in order to assess expression of genes essential in sepsis development.
“With some microbes, we have identified small, potentially therapeutic molecules that stop the production of an important toxin by understanding the important microbial pathways that turn on toxins and cause the host problems,” DiRita explained. “This next generation of antibiotics won’t kill bacteria – they will protect it from being lethal.”
The Hammer lab aims to limit the infectious capacity of the Gram-positive pathogen methicillin-resistant Staphylococcus aureus (MRSA) by screening MSU’s growing library of new plant-based compounds for ones that will inhibit its metabolic pathways.
“Through our research, we know that S. aureus has an interesting pathway of becoming resistant to several classes of antibiotics – it switches its metabolism to a small colony variant, or SCV,” Hammer said. “This is somewhat good news because our work, and work done by many other labs, demonstrated that S. aureus only uses two metabolic pathways to proliferate during infection, aerobic respiration and fermentation. SCV’s rely on fermentation.”
Metabolically speaking, S. aureus is somewhat similar to humans. When we exercise, oxygen becomes limited and lactic acid is produced via fermentation – hence sore muscles. S. aureus, in SCV form, also makes lactic acid as a fermentative end-product.
“We can force S. aureus into a fermentative, SCV state with a class of drug treatment called aminoglycocides,” Hammer said. “My research program is interested in finding compounds in our chemical library that selectively kill these SCVs to design a combinatorial therapy that potentiates the activity of the aminoglycocides.”
“Fundamentally, we are biologists who are curious about bacteria and how they work and, if they are harming people, how we can stop them from working,” DiRita added. “If this is a space race, we are John Glenn circling the earth. These are the early days for this type of research, and MSU, thanks to the MSU Foundation, is leading the way.”
BMB graduate student Garrett Miller working in the Hamberger Lab and Rajab Curtis, a master’s student in the College of Veterinary Medicine working with the DiRita and Hammer Labs, are also part of the study.
* Centers for Disease Control



 Print
Print Email
Email